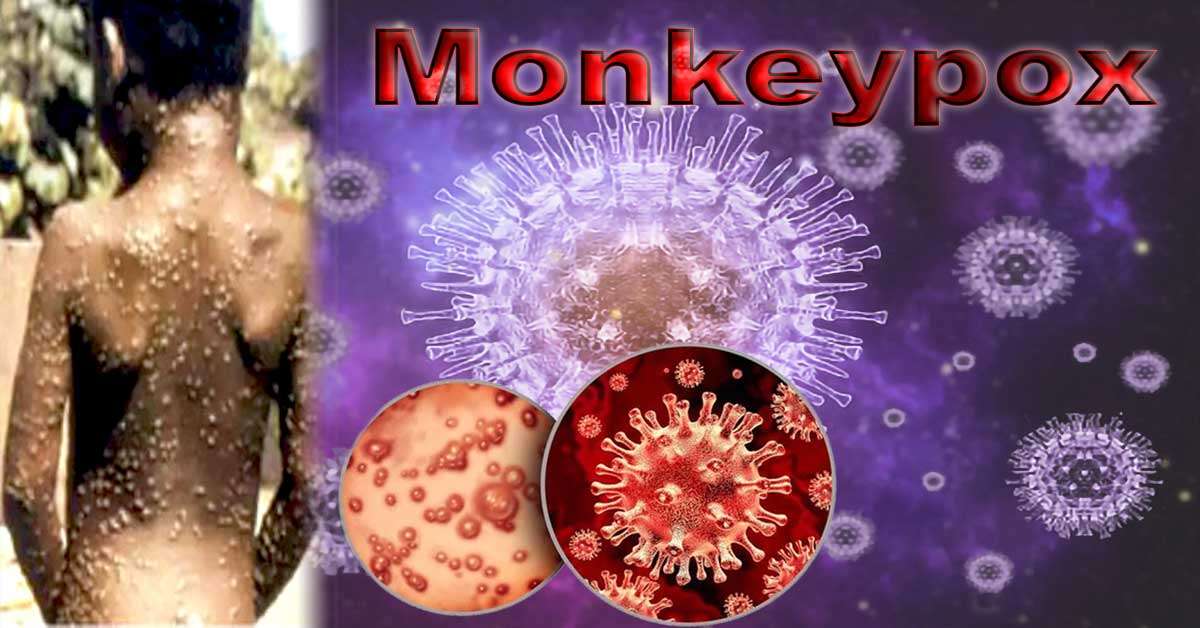
Do you want to know about the Monkeypox virus? Is it dangerous or not? What are the signs, symptoms, and pathophysiology of Monkeypox? Monkeypox is a less dangerous viral zoonosis than smallpox (a virus that spreads from animals to people). It shares symptoms and signs with smallpox. Since smallpox was eradicated in 1980 and vaccinations were subsequently discontinued, Monkeypox has become public health’s most significant orthopoxvirus. Primarily found in central and western Africa, monkeypox spreads to urban areas and is frequently found near tropical rainforests. Numerous species inhabit rodents and primates that are not humans.
The monkeypox virus consists of two DNA strands and an envelope. It belongs to the Poxviridae family and the Orthopoxvirus genus. The virus that causes monkeypox has two distinct genetic groups—the clade of central Africa (Congo Basin) and the clade of west Africa—in the past, believed that the Congo Basin clade was more contagious and caused more severe illness. The country where both virus clades have been discovered in Cameroon. It is also the only country that geographically separates the two groups.
Monkeys are the natural host for the monkeypox virus. Multiple animal species have been discovered to be susceptible to the monkeypox virus. It includes non-human species such as dormice, rope and tree squirrels, and Gambian pouched rats. The natural history of the monkeypox virus is still unclear, and additional research is required to identify the virus’s reservoir(s) and determine how it spreads in the wild.
Monkeypox Outbreaks
The Democratic Republic of the Congo, which had declared smallpox eradicated in 1968, confirmed the discovery of human monkeypox in a 9-month-old boy. More and more cases of illness have been reported in central and western Africa ever since. The majority of these outbreaks start in rural rainforest areas of the Congo Basin, especially in the Democratic Republic of the Congo.
Since it affects people worldwide, not just in west and central Africa, monkeypox is an important disease for global public health. The United States experienced the first monkeypox outbreak outside of Africa in 2003. Pet prairie dogs infected with the disease were responsible. These animals were kept alongside imported dormice and pouched rats from Ghana and the Gambia.
This outbreak in the United States caused over 70 cases of monkeypox. Monkeypox was detected in travelers from Nigeria to Israel in September 2018, the UK in September 2018, December 2019, May 2021, and May 2022, Singapore in May 2019, and the United States in July and November 2021. In May 2022, monkeypox was discovered in several countries where it was uncommon. Currently, research is being conducted to learn more about the disease’s source, origin, and spread.
Difference between chickenpox and smallpox
Some symptoms of Monkeypox are identical to those of smallpox, a now-extinct orthopoxvirus infection closely related to Monkeypox. About 30% of those who contracted smallpox perished from it, making it more lethal and contagious.
Vaccination programs in west and central Africa have reduced the spread of Monkeypox, making it more likely for unvaccinated people to contract the disease.
Even though smallpox is no longer a naturally occurring disease, the global health community remains on high alert if it reappears due to natural causes, laboratory error, or intentional release. New vaccines, diagnostic tests, and antiviral medications are being developed to ensure that the world is prepared for the return of smallpox. These may be useful for preventing and treating Monkeypox.
Monkeypox transmission
Zoonotic transmission can occur when a person comes into direct contact with an infected animal’s blood, body fluids, skin, or mucosal lesions. Numerous animals in Africa, including rope squirrels, tree squirrels, Gambian pouched rats, dormice, and various species of monkeys, have exhibited signs of monkeypox infection. People living in or near forests may be exposed to sick animals in a limited or indirect manner.
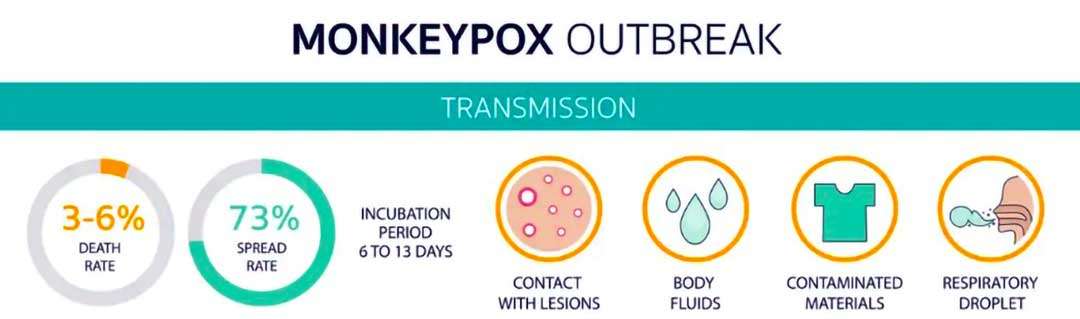
Human-to-human transmission can occur when a person’s secretions, skin sores, or recently contaminated objects come into close contact with another person. Because respiratory droplet particles require prolonged face-to-face contact, health workers, family members, and other close contacts of active cases are more likely to become ill.
Monkeypox transmission period
It typically takes between 6 and 13 days for Monkeypox to spread, but symptoms can appear between 5 and 21 days later. The duration of a typical case of monkeypox is between two and four weeks. Children are more likely to have severe cases, depending on the amount of virus they were exposed to, their health, and any complications they experienced. In the past, the death rate from Monkeypox ranged from 0% to 11% of the general population but was significantly higher among young children. Recent case fatality rates have ranged between 3 and 6 percent.
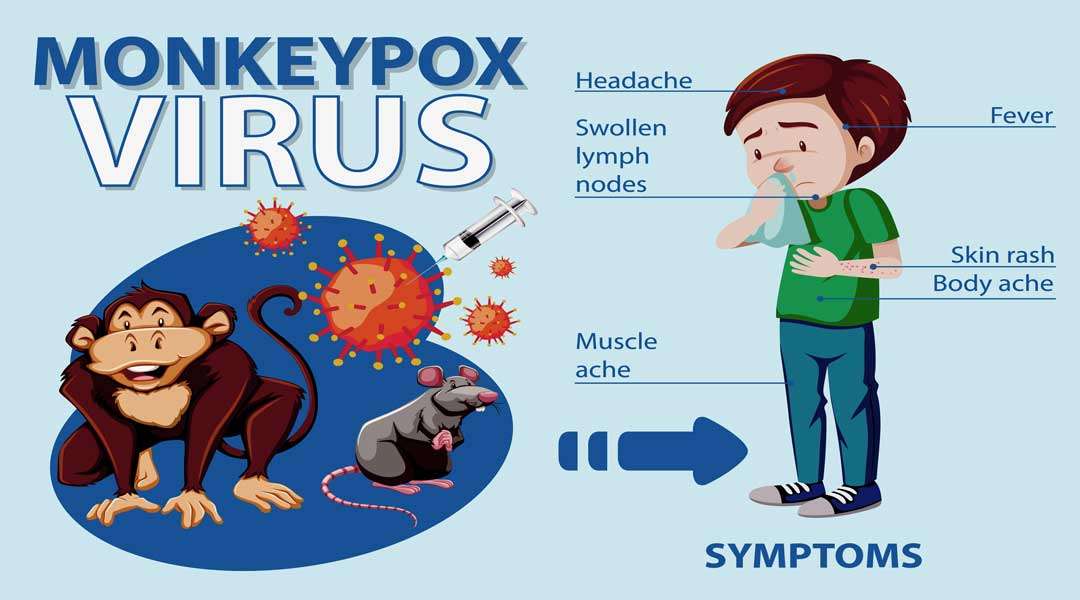
Monkeypox symptoms
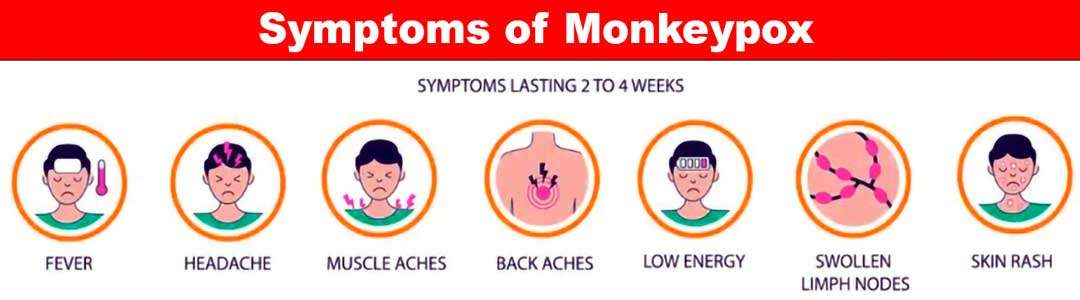
The infection has two phases: the invasion phase, which lasts between 0 and 5 days and is characterized by fever, severe pain in the head, lymphadenopathy (swelling of the lymph nodes), back pain, myalgia (muscle aches), and severe case of asthenia (lack of energy). Lymphadenopathy is a characteristic of Monkeypox that distinguishes it from other diseases that may appear similar (chickenpox, measles, smallpox)
- Typically, the rash appears one to three days after the onset of a fever. Typically, the rash appears on the face and extremities rather than the trunk. Additionally, it affects the oral mucous membranes, genitalia, and conjunctiva.
The rash progresses from macules, which are flat, firm spots, to papules, which are slightly raised, firm spots, to vesicles, which are fluid-filled clear spots, to pustules, which are yellow fluid-filled spots, to crusts that dry up and fall off.
If the immune system was compromised, the outcomes could be worse. People under 40 or 50 (depending on the country) may now be at a greater risk of contracting Monkeypox because smallpox vaccination campaigns have been discontinued everywhere since the disease was eradicated.
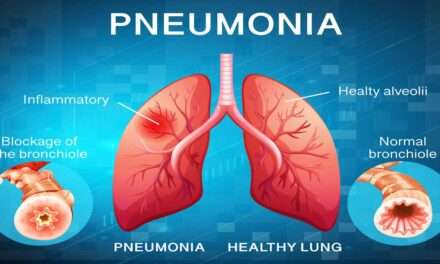
Monkeypox can cause complications such as secondary infections, bronchopneumonia, sepsis, encephalitis, and corneal infections that result in vision loss. No one knows how prevalent an infection without symptoms may be.
Diagnosis of Monkeypox
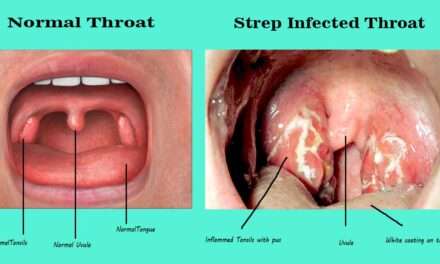
Other rash illnesses, such as chickenpox, measles, bacterial skin infections, scabies, syphilis, and medication-related allergies, must be considered when making a clinical differential diagnosis. In the early stages of the disease, lymphadenopathy can help physicians distinguish between Monkeypox, chickenpox, and smallpox.
If Monkeypox is suspected, health professionals must collect and transport the sample to a lab with the appropriate equipment. Specimens should be packaged and shipped following local, state, and federal regulations.
Polymerase chain reaction (PCR) is the most accurate and sensitive laboratory test. Lesions on the skin, such as dry crusts and the fluid from vesicles and pustules, provide the best samples for diagnosing Monkeypox.
A biopsy can be performed. Lesions samples must be kept cold and stored in a dry, sterile tube without a virus-transporting medium.
Due to the serological cross-reactivity of orthopoxviruses, testing for antigens and antibodies cannot confirm that a person has Monkeypox. When resources are limited, serology and antigen detection methods should not be used to diagnose or investigate a case.
In addition, individuals vaccinated with a vaccinia-based vaccine recently or in the past (for instance, anyone vaccinated before smallpox was eradicated or more recently due to a higher risk, such as orthopoxvirus lab workers) may produce false positive results.
To determine the significance of the test results, the following patient information must be included with the specimens:
- Age.
- Date fever began.
- Which date sample was collected?
- Date of patient’s current condition (stage of rash).
- The date rash began.
Therapeutics for Monkeypox
Clinical care must be fully optimized to effectively treat monkeypox symptoms, deal with complications, and prevent long-term effects. Patients should be provided with fluids and food to maintain their nutritional health. Recurring bacterial infections should be treated as necessary.
Vaccination Multiple observational studies have demonstrated that the smallpox vaccine prevents monkeypox approximately 85 percent of the time. If you have previously been vaccinated against smallpox, you may experience a milder illness.
Most people who have received a smallpox vaccination have a scar on their upper arm. The first generation of smallpox vaccines is no longer available to the general public. Some laboratory or healthcare workers may have been vaccinated against smallpox more recently to prevent occupational exposure to orthopoxvirus.
A brand-new vaccine against monkeypox was authorized in 2019. It comprises the Ankara strain of the attenuated, modified vaccinia virus. This vaccine must be administered twice but has yet to be completely available. Vaccines for both smallpox and monkeypox are derived from the vaccinia virus. It is because the vaccinia virus also protects the immune response to orthopoxviruses.
Monkeypox Prevention
The most effective method for preventing the spread of monkeypox is to make people aware of the risk factors and teach them how to limit their exposure to the virus.
Reducing the likelihood of transmission from one person to another to prevent an outbreak from spreading, it is crucial to keep an eye on it and locate cases as soon as possible. During an outbreak of human monkeypox, the most common way to contract the virus is through close contact with an infected individual.
Household members and healthcare professionals are more susceptible to illness. When caring for patients with a suspected or confirmed monkeypox virus infection or when handling samples from these patients, healthcare professionals should take the necessary precautions to prevent infection. The best caregivers are those who have received a smallpox vaccination.
Human and animal samples that may have been exposed to the monkeypox virus should only be handled by individuals trained to do so and to work in properly equipped laboratories. Patient specimens must be triple-packaged following the WHO’s recommendations for transporting infectious substances safely.
Reducing the likelihood of animal disease transmission
Most human infections have been transmitted from animals to humans over time. It is important to avoid unprotected contact with wild animals, especially sick or dead ones, and their meat, blood, and other byproducts. All foods containing meat or animal parts must be fully cooked before consumption.
Monkeypox can be prevented by restricting animal trade.
Some countries have restrictions on the number of primates and rodents that can be imported. Immediately, captive animals suspected of having Monkeypox should be quarantined and isolated from other animals. Animals that may have been in contact with an infected animal must be kept in quarantine for 30 days, handled safely, and watched for signs of Monkeypox.