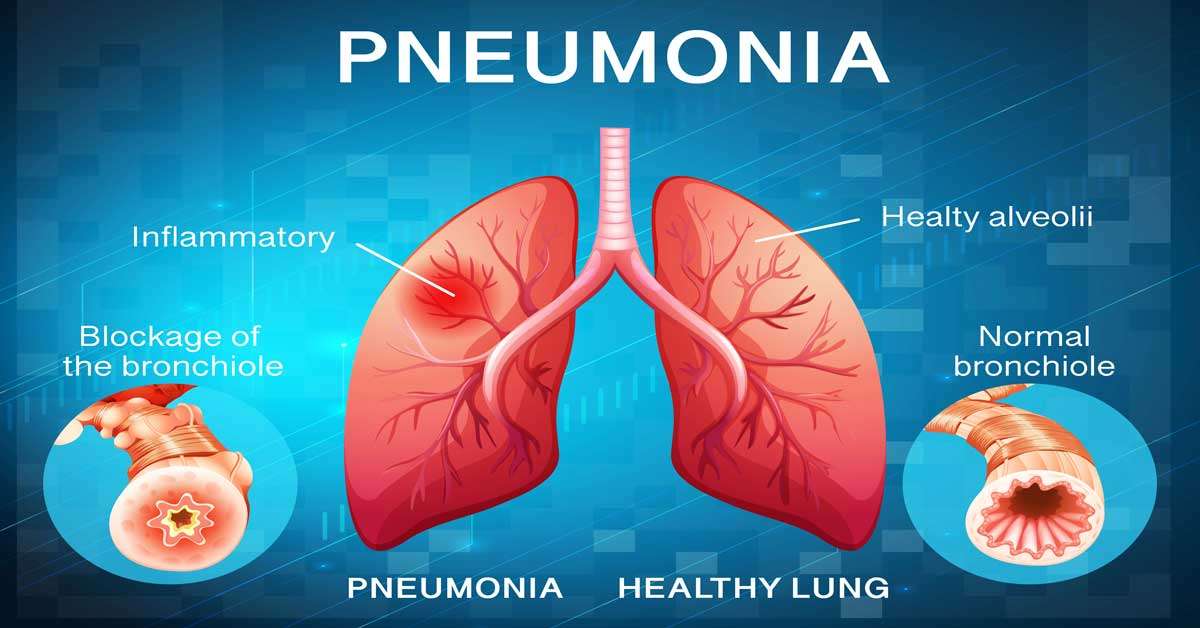
Are you ready to learn about the lethal disease Pneumonia? How it spreads, and what are the signs and symptoms? Is this can be cured with medicine? Does Pneumonia have the vaccine or not? Then give your time to complete reading this article.
As the leading cause of missed workdays in the general population, respiratory tract infections are more common than other organ infections. Most are viral upper respiratory tract infections (common cold, pharyngitis). Still, lung infections caused by bacteria, viruses, mycoplasma, and fungi continue to cause death in the United States, accounting for 2.3% of all fatalities. The extremely broad definition of this disease encompasses any infection of the lung parenchyma.
It may develop if local defense systems or the host’s systemic resistance are compromised. Deficiencies in humoral and innate immunity, including neutrophil and complement deficiencies, typically cause a rise in pyogenic bacterial infections. Cell-mediated immune deficiencies cause an increase in infections with intracellular microorganisms such as mycobacteria and herpesviruses. Chronic illnesses, immune system deficiencies, immunosuppressive drug use, and leukopenia are all factors that affect overall resistance.
Is pneumonia contagious?
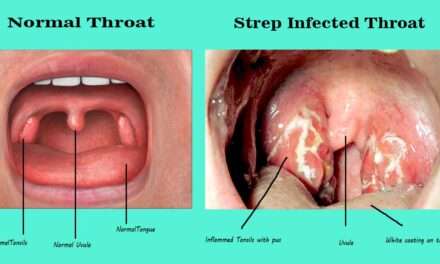
Although the viruses and bacteria that cause upper respiratory tract pneumonias are contagious, it is themselves not. Contagious pneumonia is a form of pneumonia that spreads from person to person. Most pneumonitis cases are spread through coughing, sneezing, or talking, which causes respiratory droplets to be released into the air. These droplets can be inhaled if they come into closeness. Less commonly, it can be transmitted by touching one’s mouth or nose after contacting an infected object. Some people easily develop this disease, and not everyone who is exposed to the disease will get it.
When you have pneumonia, the duration of your contagious period is unpredictable. The time it takes to spread to others is determined by the type of disease you have and what causes it. If you have a bacterial infection and start taking antibiotics after your fever has subsided, you are usually infectious for 48 hours. If viral infection occurs, the contagious period shortens as symptoms, particularly fever, resolve. Pneumonia caused by fungi is not contagious.
Types of pneumonia
Community-Acquired Bacterial Pneumonias
Acute pneumonia acquired from the general environment in otherwise healthy people is known as community-acquired pneumonia (in contrast to hospital-acquired pneumonia). It could be viral or bacterial. Clinical and radiologic characteristics are frequently insufficient to differentiate them. Several newer biomarkers for identifying patients with bacterial infections and predicting their prognosis have been developed. Bacterial infections are associated with significantly higher levels of the acute-phase reactants C-reactive protein and procalcitonin, primarily produced by the liver.

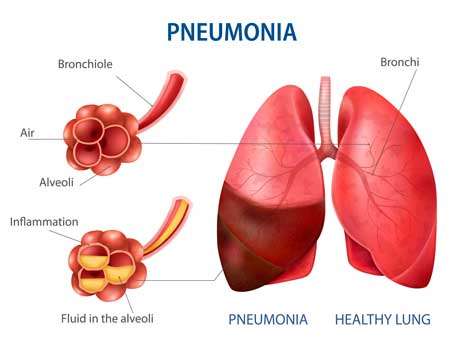
A bacterial upper respiratory tract infection frequently follows a viral upper respiratory tract infection. The accumulation of inflammatory exudate in the alveoli caused by bacterial invasion of the lung parenchyma causes pulmonary tissue consolidation (or “solidification”). Various factors, including the etiologic agent, the host’s response, and the degree of involvement, determine the specific type of pneumonia.
Risk factors include advanced age, chronic conditions (such as diabetes, congestive heart failure, and COPD), congenital or acquired immune deficiencies, and diminished or absent splenic function (sickle cell disease or post-splenectomy, which puts the patient at risk for infection with encapsulated bacteria such as pneumococcus).
- Bacteria: The most common cause of CAP is infection with the Streptococcus bacteria, also known as pneumococcal disease. Meningitis, sinus infections, and ear infections can all be caused by pneumococcal disease. Atypical pneumonia is caused by the bacterium Mycoplasma pneumonia and typically manifests with milder symptoms. Haemophilus influenza, Chlamydia pneumonia, and Legionella (which causes Legionnaires’ disease) are other bacteria that cause CAP.
- Viruses: The viruses that cause the common cold, influenza (the flu), COVID-19, and respiratory syncytial virus can all cause disease on rare occasions (RSV).
- Fungi (molds): Rare causes of infection include Cryptococcus, Pneumocystis jirovecii, and Coccidioides. WeakPeople with weakened immune systems are more likely to contract fungus-caused pneumonia.
- Protozoa: Toxoplasma and other protozoa are rare causes of ilness.
Health Care-Associated Pneumonia
It is linked to healthcare, According to recent research, it is a distinct clinical entity with significant risk factors. These include current intravenous antibiotic therapy, chemotherapy, or wound care, at least two days in the hospital, presentation from a nursing home or long-term care facility, and attendance at a hospital or hemodialysis clinic. The most commonly isolated microorganisms are Pseudomonas aeruginosa and methicillin-resistant Staphylococcus aureus. Compared to community-acquired pneumonia, these patients have a higher mortality rate.
Hospital-acquired Pneumonia
Pneumonias contracted during a hospital stay are known as hospital-acquired pneumonia. Patients with severe underlying diseases, immunosuppression, long-term antibiotic therapy, or invasive access devices, such as intravascular catheters, are more likely to develop them. Patients who require mechanical ventilation are especially vulnerable.
A hospital-acquired infection is a serious, often fatal complication caused by a pre-existing condition (that led to hospitalization). The most common isolates are gram-positive cocci (primarily S. aureus and S. pneumonia) and gram-negative rods (Enterobacteriaceae and Pseudomonas species). Similar organisms have been isolated in ventilator-associated lung infections, but gram-negative bacilli are more common.
Ventilator-acquired Pneumonia
You risk developing ventilator-associated pneumonia (VAP) if you require a respirator or other breathing aid while receiving medical care (typically in the intensive care unit). The same bacteria that cause both hospital-acquired and community-acquired pneumonia cause VAP.

Chronic Pneumonia
It is a localized lesion involving one or more lymph nodes in immunocompetent patients. Bacteria (such as M. tuberculosis) or fungi are usually blamed for the granulomatous inflammatory response (e.g., Histoplasma capsulatum). This article discusses fungal-caused chronic pneumonia.
Histoplasmosis
Inhaling dust contaminated with bird or bat droppings, which contains microscopic spores (microconidia), the infectious form of the fungus, and causes infection with Histoplasma capsulatum. It is only found in the Caribbean, Ohio, and Mississippi rivers. It is also found in Australia, Mexico, Central and South America, and parts of Eastern and Southern Europe, Africa, and East Asia. Histoplasmosis can be diagnosed by culture or by identifying the fungus in tissue lesions. Serologic tests for antigens and antibodies are also available.
Blastomycosis
Blastomyces dermatitidis is a soil-dwelling dimorphic fungus. In addition to the central and southeast United States, infectious disease has spread to Canada, Mexico, the Middle East, Africa, and India. The three clinical forms are pulmonary blastomycosis, disseminated blastomycosis, and a rare primary cutaneous form caused by organism inoculation into the skin. Typical symptoms include a productive cough, headache, chest pain, loss of appetite, fever, abdominal pain, night sweats, chills, and pulmonary blastomycosis.
Coccidioidomycosis
The vast majority of people who inhale Coccidioides immitis spores become infected and develop a delayed-type hypersensitivity reaction. The skin test response rate in endemic areas of the southwestern and western US and Mexico exceeds 80%.
Pneumonia in the Immunocompromised
One of the most common and dangerous side effects in patients whose immune systems have been compromised by disease, immunosuppressive therapy for organ or hematopoietic stem cell transplants, chemotherapy for cancer, or radiation is the development of a pulmonary infiltrate, with or without symptoms of infection (such as fever). This pneumonia can be caused by various opportunistic infectious agents, many of which rarely infect healthy hosts, and multiple agents frequently cause them.
These opportunistic infections are associated with a high mortality rate. These infiltrates can have a variety of diagnoses, including drug interactions and involvement in lung cancer. They are classified into three groups based on the causative agent: (1) bacteria (P. aeruginosa, Mycobacterium species, Listeria monocytogenes, and L. pneumophila), (2) viruses (cytomegalovirus [CMV], and herpesvirus), and (3) fungi (P. jiroveci, Candida species, Aspergillus species, the Phycomycetes, and Cryptococcus neoformans)
Symptoms of pneumonia in adults
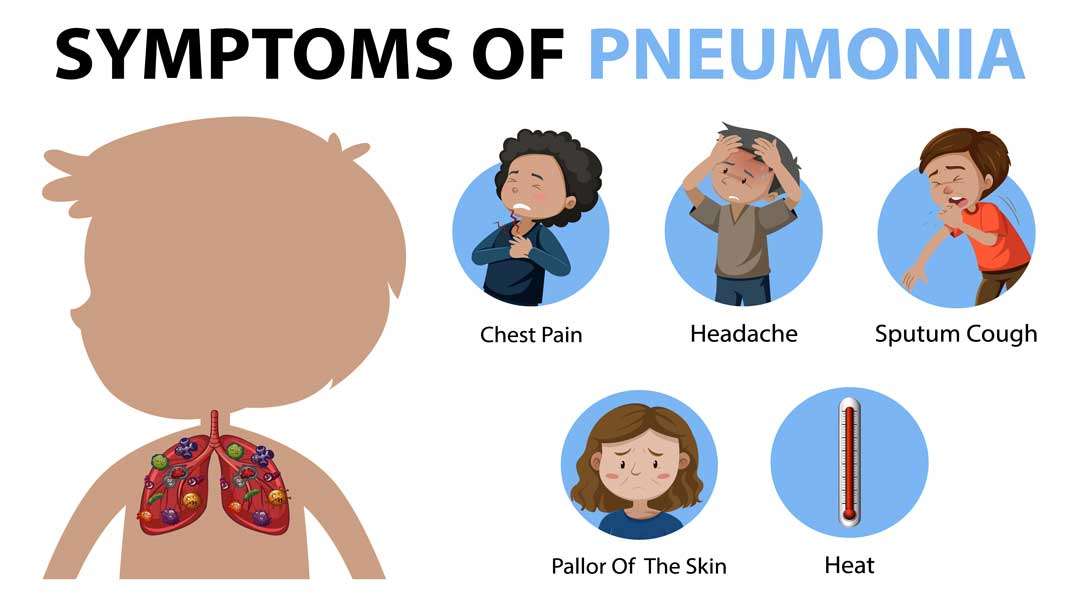
Symptoms range from mild to severe. Infants, young children, and the elderly may exhibit various symptoms.
Bacterial pneumonia Symptoms
Bacterial pneumonia symptoms can appear gradually or suddenly. The following symptoms are present: (up to 40.55 degrees Celsius or 105 degrees Fahrenheit).
- Cough up mucus that is yellow, green, or blood-colored.
- Fatigue (Tiredness).
- Rapid respiration
- Difficulties breathing.
- Quick heartbeat
- Shivering or sweating.
- Chest or abdominal pain, particularly when coughing or deeply inhaling.
- A decrease in appetite.
- Lips, skin, or nails that are pale (cyanosis).
- Dizziness or altered mental state.
Symptoms of viral pneumonia
Symptoms of viral pneumonia usually appear within a few days. Along with symptoms similar to bacterial pneumonia, you may also experience the following:
- Migraine.
- Muscle aches.
- Extreme exhaustion or weakness.
How to Avoid Getting Infectious Pneumonia
Cover Your Mouth and Nose
Although covering your mouth with a tissue when coughing or sneezing is advised, not everyone can reach a tissue in time. When you need to cough or sneeze but don’t have a tissue, use your elbow to cover your mouth or nose. Coughing or sneezing into your elbow reduces the likelihood of spreading your infection to door handles, faucets, or anything else you touch.
Wash Your Hands
Regardless of your current state of health, hand-washing with soap and water is frequently beneficial to your health. When you wash your hands after getting sick, you reduce the germs you can spread. Maintaining good health and washing your hands reduces the chances of exposing your body to harmful germs.
Limit Your Social Contacts
Limiting contact with others is one of the best things you can do while recovering from pneumonia. The COVID-19 pandemic has taught us that keeping at least six feet away from people reduces their exposure to viral or bacterial particles when we breathe or speak. COVID-19 has the potential to cause viral pneumonia.
In the United States, four pneumococcal vaccines are currently available. Children under the age of two, adults over 65, and people of any age who are immunocompromised or have certain chronic health conditions should all receive one of these vaccines, according to the Centers for Disease Control and Prevention organization (CDC).
Treatment
Vaccination is the best and safe way to prevent various types of bacterial Pneumonia. Many over-the-counter cold and flu medications may not provide complete symptom relief. Your doctor prescribes antibiotics. As a result, you should start feeling better in a few days. Inform your family doctor if you are taking or plan to take any other medications. Take rest as much as possible and drink plenty of liquids.
Pneumococcal Vaccines
There are two types of pneumococcal vaccines:
Pneumococcal polysaccharide vaccine (PCV13, PCV15, and PCV20); (PPSV23)
- The influenza vaccine: According to Dr. McGinniss, the influenza vaccine is extremely effective at preventing bacterial pneumonia as a secondary infection because influenza increases your risk of bacterial pneumonia. Dr. McGinniss said that this vaccine could also help prevent influenza-caused viral pneumonia.
- Pneumococcal vaccines: The pneumococcal conjugate vaccine (PCV13) and the pneumococcal polysaccharide vaccine are two vaccines used to prevent infections caused by pneumococcus bacteria, the most common type of bacteria responsible for pneumonia (PPSV23). These are typically advised for adults 65 and older, those suffering from chronic illnesses, and smokers. Dr. Panettieri believes that current vaccines are extremely effective.
- Hib vaccine: “Hib” is an abbreviation for the bacterium Haemophilus influenza type B, which can cause meningitis and pneumonia. According to the NHLBI, it is given to neonates as young as two months old and is recommended for all children under five in the United States.
- The COVID-19 vaccine: Despite the vaccines’ recent development, Dr. Mc Ginniss noted that they had been shown to reduce the risk of contracting a severe form of the virus, which can cause life-threatening complications such as pneumonia.
CDC’s Pneumococcal Vaccine Recommendations
CDC Recommendations for Pneumococcal Vaccine PCV13 (Prevnar 13), which protects against 13 types of bacterial pneumonia, is recommended for:
- Four-part series for young children (under two years old). This vaccination should be given to them at ages 2, 4, 6, and 12 to 15 months.
- Children and adolescents between the ages of 2 and 18 who have specific medical conditions
PCV15 (Vaxneuvance) or PCV20 (Prevnar 20) are recommended to protect against 15 and 20 types of bacterial pneumonia, respectively.
- People over the age of 65
- Adults between the ages of 19 and 64 who have specific health issues or risk factors
The PPSV23 (Pneumovax23) vaccine, which protects against 23 different types of bacterial pneumonia, is recommended in the following situations:
- Children and adolescents between the ages of 2 and 18 who have specific medical conditions
- People over the age of 19 who receive PCV15 or PCV13
Remember that PCV15 and PCV20 are brand new, with usage instructions published in January 2022. Adults who previously received the older PCV13 vaccination should receive a PPSV23 vaccination (or PCV20 if PPSV23 is unavailable).