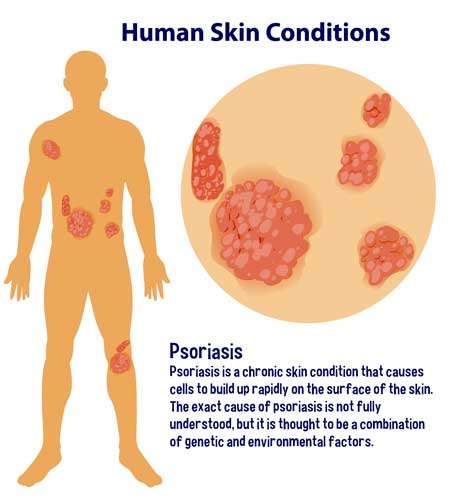
Do you want to learn more about psoriasis? Explain the cause. Is it curable or incurable? Then carefully read this article. We will offer advice on psoriasis prevention and treatment. This relapsing, persistent, or chronic skin condition is characterized by scaling. Individual lesions have a distinct appearance: they are erythematous, have sharp margins, and are covered in silvery scales. Psoriatic patients’ clinical presentations vary greatly, but most have few fixed plaques.
In other words, It is a skin disease characterized by an autoimmune, inflammatory dermatosis that persists. It affects 2% to 3% of the global population, 2.2% of Americans, and varying proportions of people from different cultures. Northern Europe has the highest psoriatic prevalence globally, while Eastern Asia has the lowest.
An arthritic condition affects 15% of psoriatic patients. Psoriatic arthritis can cause mild to severe joint deformities that resemble rheumatoid arthritis. The condition can affect any joint in the body and can be unilateral or symmetrical. HIV, myopathy, and enteropathy are all linked to this disease.
Pathophysiology Psoriasis
Psoriasis is caused by genetic and environmental factors interacting. It is linked to genes in the HLA locus, as are many other autoimmune diseases. T cells can create an abnormal microenvironment by releasing cytokines and growth factors. These substances promote keratinocyte proliferation and result in distinct lesions. Interactions between CD4+vT cells, vCD8+ T cells, dendritic cells, and keratinocytes produce a cytokine “soup” dominated by TH1 and TH17 cytokines like IL-12, interferon, tumor necrosis factor (TNF), and IL-17.
The generally positive clinical outcomes observed in TNF inhibitor-treated patients serve as a reminder of the significance of these factors. Furthermore, lymphocytes provide growth factors to keratinocytes, which may aid in epidermis thickening. The Koebner phenomenon describes susceptible individuals’ propensity to develop psoriatic lesions in response to local trauma. Local trauma is thought to cause a self-replicating inflammatory response.
Epidemiology of Psoriasis
It affects between 1% and 2% of both sexes in most ethnic groups. The third decade is the most common age of onset, but It has been observed in infants and even a centenarian. Several lines of research have shown that genetic factors play a role in developing this disease. Its concordance is high in monozygotic twins, which is more common in affected individuals’ relatives.
Psoriatic patients have higher levels of specific class-I alleles of major histocompatibility complex gene products (MHC). It is more than a genetic disorder; some susceptible people never develop the disease’s defining lesions. Numerous environmental factors, such as infection, physical injury, stress, and drugs, can trigger psoriatic disorder in susceptible individuals.
Symptoms of Psoriasis
Psoriatic disorder symptoms include:
• Small, scaly patches (common in children);
• Dry, cracked skin that may bleed; and
• Itching, burning, or discomfort.
• Rash that varies in color, primarily purple with the grayscale on brown or black skin and pink or red with the silver scale on white skin.
Types of Psoriasis
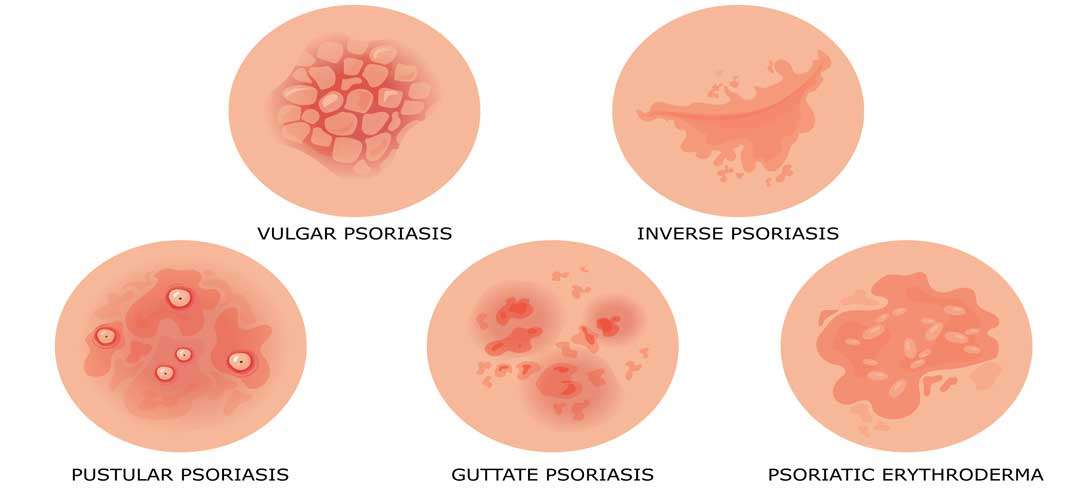
There are various types of psoriasis, each with its own set of signs and symptoms:
Plaque of psoriasis: is the most common type, is distinguished by scale-covered, dry, raised skin patches (plaques). They could be scarce or plentiful. The scalp, lower back, elbows, and knees are common sites. The patches are assigned different colors based on the color of the patient’s skin. A brown or black skin wound may heal with temporary color changes (post-inflammatory hyperpigmentation).
Nail psoriasis: can cause pitting, irregular nail growth, and discoloration of the fingernails and toes, and nails may become loose and detached from the nail bed (onycholysis). The nail may break depending on the severity of the disease.
Guttate psoriasis: most commonly affects young adults and children. The common cause is a bacterial infection, such as strep throat. Small, drop-shaped, scaly lesions on the trunk, arms, and legs distinguish it.
Inverse psoriasis: The breast’s groin, buttocks, and skin folds are the most commonly affected areas by inverse psoriasis. It results in scaly, irritated skin patches that worsen with friction and sweat. Fungi may be to blame for this type of disorder.
Pustular psoriasis: Pus-filled blisters distinguish psoriasis from pustules, A rare form of pustular psoriasis. It can manifest as small or large patches on the palms or soles.
Erythrodermic psoriasis: associated with erythroderma. The least common form of psoriasis, erythrodermic psoriasis, can cause a peeling rash that can itch or burn intensely and cover the entire body. It can be acute (of short duration) or chronic (of long duration) (chronic).
Causes of Psoriasis
Physical Factors: These physical conditions can cause psoriatic disease. Cuts, scrapes, insect bites, abrasions, lacerations, burns, sunburn, contusions, insect bites, surgical incisions, and other skin injury conditions are common, particularly in cold and dry weather. Infections can also result in HIV infection, Streptococcal pharyngitis, and viral bronchitis.

Medication is essential in the treatment of this problem. Antimalarial medications, B-adrenergic blockers, corticosteroid withdrawal, and lithium exposure can cause this issue in people of any gender. For many years, ultraviolet light has been used successfully to treat this problem. It is only worsens when exposed to toxic doses of UV light.
Psoriasis triggers
Many psoriatic-prone people may go years without experiencing symptoms before an environmental factor triggers the disease. It is commonly triggered by infections such as strep throat, skin infections, cold, dry weather—consumption of excessive alcohol; smoking and smoking exposure; blood pressure medicines, and antimalarial drugs.
Locations of Psoriasis
The type of this disease you have will be treated and addressed by your medical team, and the kind of treatment you receive will be determined by where it appears on your body. Download our free guide to learn how to care for your psoriatic-affected skin. Here are some common symptoms and an overview of the five distinct types.

Psoriasis of the genitalia
Psoriasis genitals are very common. At some level in their lives, up to two-thirds of patients will develop genital psoriatic. The genital region, as well as the inner and upper thighs, can be affected.
Psoriasis of scalp
Over 60% of people who have psoriatic disorder also have scalp psoriasis. The whole skin around the ears, hairline, forehead, and back of the neck can all be affected.
Facial Psoriasis
Fifty percent of people with psoriatic disorder also have facial psoriasis. Any part of the face can affect the brows, the skin between the upper lip and nose, and the upper forehead.
Hands, feet, and nails
It can also affect the hands, feet, and nails. Palmoplantar psoriasis is a type of psoriatic disorder that affects the palms and soles of the feet (PPP). Palmoplantar psoriasis affects 12 to 16 percent of psoratic patients. Furthermore, 50% of psoriasis patients may have nail changes.
Psoriasis can also affect the skin folds on the breasts and beneath the arms. Rubbing and sweating irritate these areas.
Diagnosis of Psoriasis
Psoriasis is usually easy to diagnose, especially if you have plaques on your scalp, ears, elbows, knees, navel, or nails. Your doctor will perform a thorough physical examination and inquire about any family members with psoriatic disease—lab tests to ensure you do not have a skin infection. The doctor performs a biopsy, which involves removing and analyzing a small skin sample. There are no other tests available to confirm or rule out psoriatic disorder.
Psoriasis Treatment
Light therapy: is one of the treatments for moderate to severe psoriatic disease. To slow the growth of skin cells, your doctor will expose your skin to ultraviolet light. Psoralen medication and a specific type of ultraviolet light are used in the PUVA treatment.
Methotrexate: Methotrexate medication, because of lung, liver, and bone marrow disease risk, this medication should be used only in extreme cases. Doctors keep a close eye on their patients. You will require laboratory tests, a chest X-ray, and possibly a liver biopsy.
Retinoic acid: (vitamin A) These vitamin A pills, creams, foams, lotions, and gels fall under the category of drugs. Retinoids are not good for pregnant or breastfeeding women due to the risk of severe side effects such as congenital disabilities.
Cyclosporine: is an antibiotic. This immune suppressant medication can treat severe conditions that have not responded to other treatments. Because it can cause high blood pressure and kidney damage, your doctor will closely monitor your health while you are taking it.
Biological therapies: Inhibit the overactive immune system found in psoriasis patients. Adalimumab (Humira), brodalumab (Siliq), certolizumab pegol (Cimzia), etanercept (Enbrel), guselkumab (Tremfya), infliximab (Remicade), ixekizumab (Taltz), risankizumab-rzaa (SKYRI), risankizumab- (Stelara).
Enzyme Inhibitor: is a substance that prevents enzymes from working. Deucravacitinib (Sotyktu) and apremilast (Otezla) are two new anti-inflammatory drugs used to treat chronic inflammatory conditions like psoriasis and psoriatic arthritis. They are pills that inhibit the function of a specific enzyme, thereby slowing down other inflammatory reactions.
An aryl hydrocarbon receptor agonist(ARH): Tapinarof (Vtama) is a once-daily steroid-free topical cream that can be applied to any body part, including sensitive areas.
What You Need to Know?
Although a nutrient-dense diet cannot prevent or cure Psoriasis, it can help to alleviate some of its symptoms. Psoriasis patients may find relief by incorporating these five changes into their daily routines.
Losing excessive weight: Despite the lack of knowledge about the relationship between weight and Psoriasis, it has been proposed that losing excess weight may improve treatment efficacy. If you’re overweight, you can mitigate the effects by trying to lose weight.
Eat a heart-healthy diet: Cardiovascular-friendly eating habits, Saturated fats, found in animal products such as meat and dairy, should be avoided by psoriatic patients. Increase your omega-3 fatty acid-rich lean proteins like salmon, sardines, and shrimp. Plant sources of omega-3s, such as walnuts, flax seeds, and soybeans, are healthy alternatives to animal products. Keeping anxiety-inducing foods at bay Inflammation occurs during the development of Psoriasis.
Avoid Psoriasis triggering food: Certain foods may also aggravate inflammation. Try to improve your condition by avoiding these foods. Examples include red meat, white sugar, and packaged foods.
Avoid drinking alcohol: There could be a link between increased flare-up frequency and alcohol consumption, which can reduce risk by cutting back or quitting. If you have an alcohol use disorder, your doctor can assist you in developing a treatment plan.
Take vitamins: Vitamins should be taken into account. Many doctors believe that vitamin-rich foods are superior to vitamin supplements. Even the healthiest eaters may need help meeting their dietary needs independently. Consult your doctor about whether you should increase your vitamin intake.